Improving Health Inequities Through Our Research
by Susan Neale
Researchers at the College of Nursing have long understood that racism is a public health crisis that, along with other societal factors, has fueled health inequities for underrepresented populations.
Several of our faculty are dedicated to conducting research seeking to reduce health disparities caused by several social determinants of health and systemic racism. This research is supported by 10 National Institutes of Health (NIH) grants, six foundation grants, and three internal (university or college) awards to our faculty and doctoral students as principal investigators or co-investigators.
It is important to recognize that social factors are primary drivers of health. As Timiya Nolan, PhD, APRN-CNP, ANP-BC, explained, “It is not race that is a driver, but rather racism. Because of racism, people of color have been systematically positioned in less than ideal circumstances (e.g., difficulties meeting physical activity and nutritional recommendations, poorer access to high quality care, less likelihood of having health insurance, difficulties with patient-provider communication, medical mistrust and discrimination) in comparison to non-Hispanic whites.” These circumstances underlie a multitude of chronic diseases, including cancer, one of Nolan’s areas of research.
The stress resulting from enduring racism can have damaging effects on health, both physical and mental.
“If you are experiencing discrimination, there’s this sense of loneliness and depression,” said Kathy Wright, PhD, RN, APRN-CNS, PMHCNS-BC, whose research includes foundational work on neural processing and perceived racial discrimination.
“We have a group of outstanding faculty actively conducting innovative research on health disparities to improve health and well-being outcomes in underrepresented populations and creating meaningful change to improve racial injustice,” said College of Nursing Dean and University Chief Wellness Officer Bernadette Melnyk, PhD, APRN-CNP, FAANP, FNAP, FAAN.
Research at the college to address healthcare disparities spans across the areas of women’s health, children and youth, aging and dementia, and chronic disease prevention and self-management.
Cancer screening, early detection and survivorship
The college has several intervention research programs focused on promoting cancer screening and early detection among racial groups who have disparately lower screening and detection rates. These include a quality of life intervention for young African American breast cancer survivors in treatment (Y-AMBIENT) led by Nolan and funded by a National Cancer Institute (NIH/NCI) career development grant (see page 2). “Health disparities among African American women and cancer include diagnosis at later stages of disease and more post-treatment issues, such as poorer quality of life and greater functional deficits, than non-Hispanic whites,” Nolan said.
Karen Patricia Williams, PhD, and her research team are implementing the NIH-funded Kin KeeperSM Cancer Prevention Intervention to address breast and cervical cancer screening with African American, Latina and Arab American women. This research takes a real-world approach, reaching out to these populations through community health workers. “In the comfort of their home, in their first language women increase their health literacy learning about their personal and familial risks, how to navigate the health system and the various resources available in their communities,” Williams said.
“Intergenerational Refugee and Immigrant Cancer Screening Project,” led by Jennifer Kue, PhD, and funded by the American Cancer Society, seeks to promote screening for breast and cervical cancer among Southeast Asian refugee and immigrant populations. Kue’s study engages bilingual and bicultural community health advisors to deliver a tailored navigation cancer screening program to Cambodian, Lao and Vietnamese women. Southeast Asian women are more than twice as likely to be diagnosed with cervical cancer than white women and have seen the greatest increase in breast cancer rates than any other racial and ethnic group in the past decade. “Receiving culturally and linguistically appropriate healthcare is imperative for refugees and immigrants. Community health advisors are critical to helping refugees and immigrants navigate a system that is unable to meet the linguistic and cultural needs of a diverse America,” said Kue.
Prenatal and postpartum care
Preterm birth is serious for many reasons: it can be a cause of infant death or lead to health complications later on for surviving infants, including respiratory distress syndrome, necrotizing enterocolitis, sepsis, cerebral palsy, developmental and language delays, and long-term respiratory and cardiovascular disease.
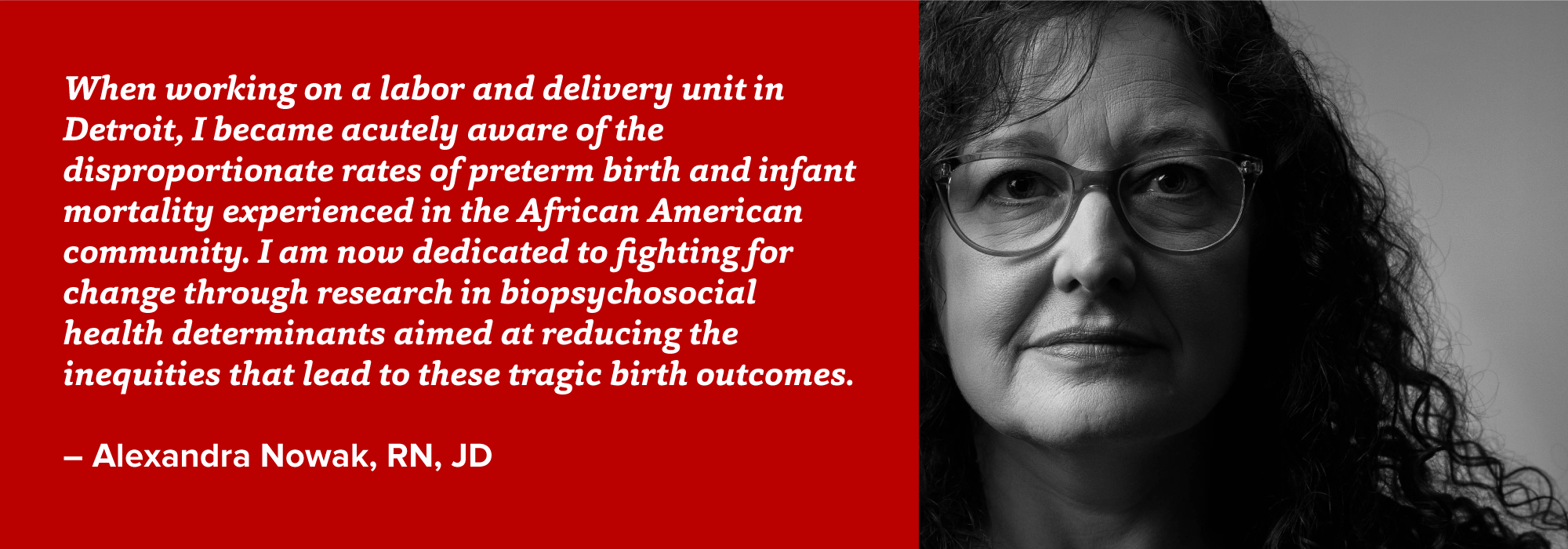
“African American women are 1.5 times more likely to have preterm birth compared with white women,” said PhD candidate Alexandra Nowak, RN, JD, whose dissertation research, funded by a National Institute of Nursing Research (NIH/NINR) F31 pre-doctoral training grant, examines the relationships among neighborhood disorder, psychological distress, DNA methylation of stress pathway genes, and gestational age at birth.
Two studies on preterm birth led by Shannon L. Gillespie, PhD, RN, “Pathways to Shortened Gestation among African American Women” and “DNA Methylation Markers of Preterm Birth Risk among Asymptomatic African American Women,” funded by the NIH, American Nurses Foundation, and Council for the Advancement of Nursing Science, consider the effects of racial discrimination as a salient stressor on the mother’s biology during pregnancy.
Cindy Anderson, PhD, APRN-CNP, ANEF, FAHA, FNAP, FAAN, is an investigator on several NIH-funded studies that examine factors such as hypertension and maternal pregnant environment that predispose African American women to premature birth.
Our researchers also look at the impact of nutrition and emotional health on prenatal and postpartum women from underrepresented populations. The research of Mei Wei Chang, PhD, RN, FAAN, focuses on prenatal and post-partum nutrition and weight control targeting socio-economically disadvantaged women. Half of the sample group for her new R-21 NIH-funded study of an intervention to prevent excessive gestational weight gain in women who are obese or overweight will be African American.
Dean Melnyk and colleagues from Boston College are implementing a National Institute of Minority Health and Health Disparities (NIH/NIMHHD)-funded clinical trial for emotionally distressed pregnant women from underrepresented racial or ethnic populations that teaches evidence-based cognitive behavioral skills to improve healthy lifestyle behaviors as well as mental and physical health outcomes. The study is enrolling pregnant women who are stressed, anxious and/or depressed in Columbus and New York City. “Given the well-established link between emotional distress, poor health and birth outcomes and the prevalence of emotional distress in these populations, prenatal care interventions designed to improve mental and physical health outcomes for these women and their children are vital,” Melnyk said.
Parenting, children and teens
Our researchers believe that it is key to include people from underrepresented populations from the beginning when designing healthcare interventions. Dianne Morrison-Beedy, PhD, RN, APRN-CNP, FAANP, FNAP, FAAN, asked Latina and African American teenagers to help her develop the Health Improvement Project for Teens (HIP Teens), a sexual wellness education program widely disseminated across the United States.
The Chicago Parent Program was developed in collaboration with parents of young African American and Latinx children. Susie Breitenstein, PhD, RN, FAAN, co-author and developer of the program, is now working on a study to test a digital adaptation. “In developing the Chicago Parent Program and the digital adaptation, we collaborated with an advisory board of mothers, fathers and grandparents who helped guide the scripts, reframe commonly used parenting principles and strategies in ways that felt more useful and relevant to them,” Breitenstein said.
Other studies to help children and youth include considering the social determinant of homelessness. “African American youth are disproportionately represented among homeless youth in Columbus as well as nationally,” said Jodi Ford, PhD, RN, FAAN, who is working on a National Institute on Drug Abuse (NIH/NIDA)-funded Housing First intervention to prevent opioid use disorder among homeless youth.

Chronic disease prevention and self-management
“African Americans are twice as likely to get Alzheimer’s disease and more likely to develop hypertension at an early age,” said Kathy Wright, PhD, RN, APRN-CNS, PMHCNS-BC. “I see the work I’m doing in hypertension as a pathway of change for many outcomes, one being cognitive – if we can decrease our blood pressure to a closer to normal range, we can reduce our risk of getting Alzheimer’s disease and other complications like stroke and chronic kidney disease that African Americans are plagued with.” Her work developing interventions for African American adults and older adults to self-manage hypertension includes mindfulness, diet and stress management tools.
A new study, “Reducing Cardiovascular Risk Factors in Black Young Adults,” funded by an NIH/NINR R01 grant and headed by Janna Stephens, PhD, RN, focuses on developing strategies and interventions to assist young African American adults who attend community colleges in creating and sustaining improved health habits in order to reduce the risk of cardiovascular issues later in life.
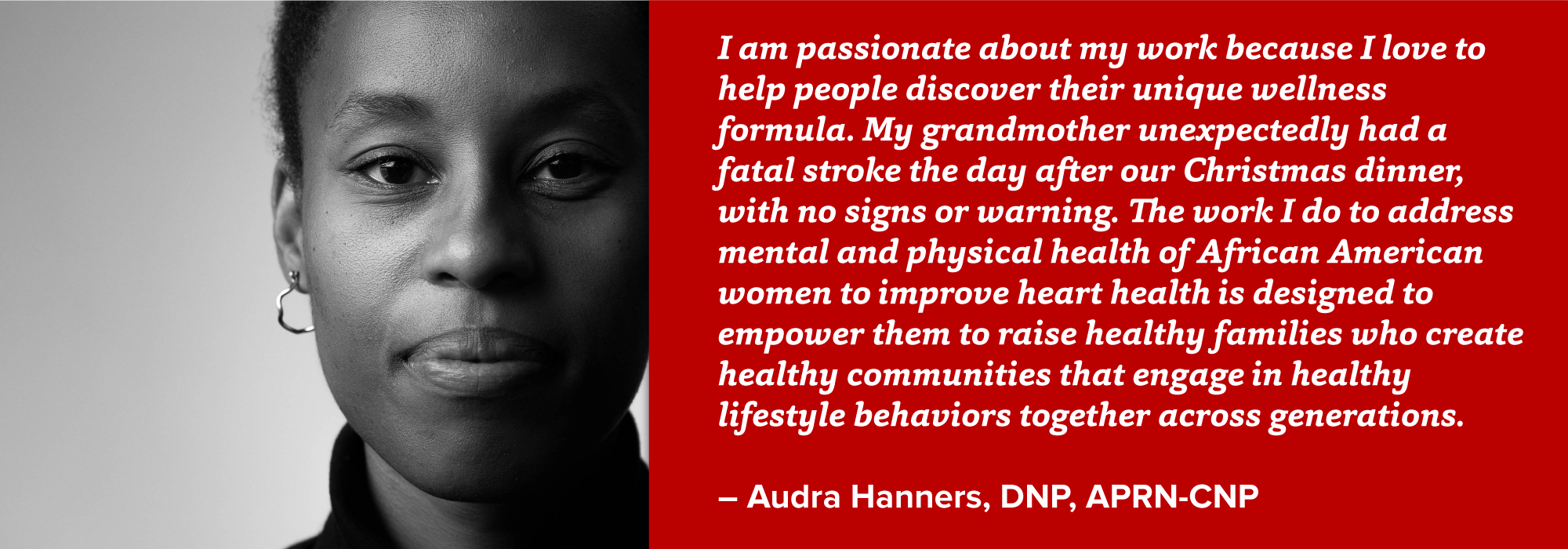
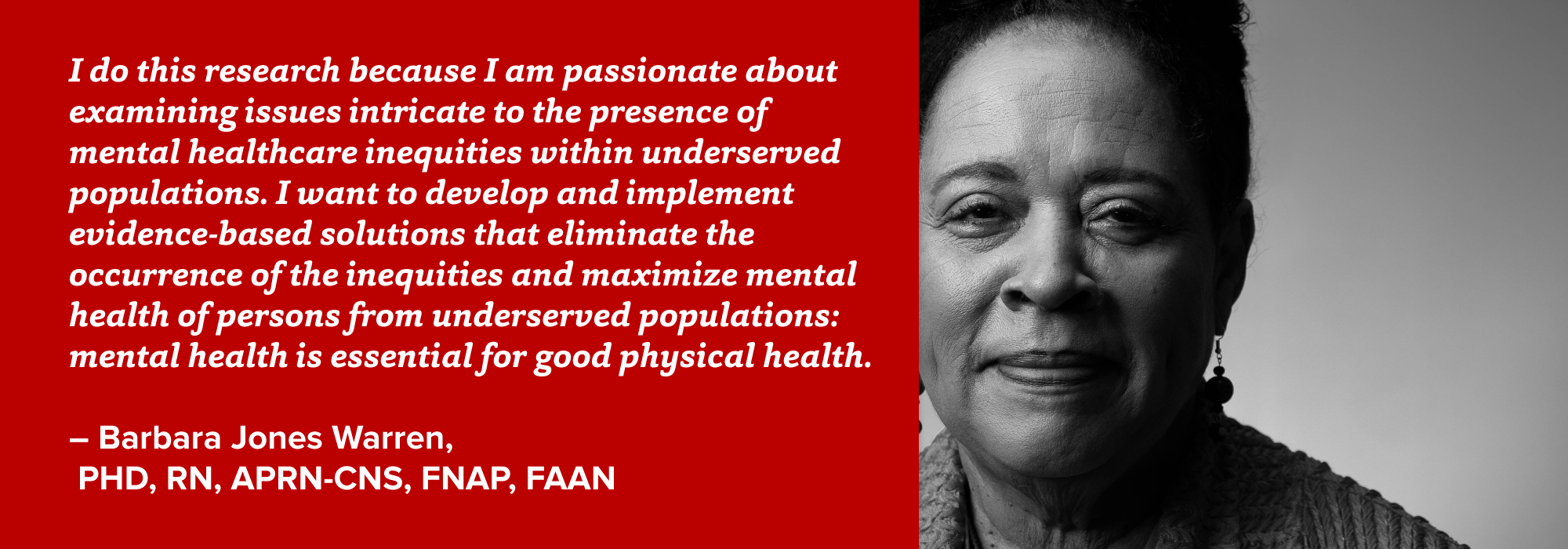
“Keto Prescribed: Translating Ketogenic Research into Clinical Practice," a health coaching program for African American women led by Barbara Jones Warren, PhD, RN, APRN-CNS, FNAP, FAAN, and Audra Hanners, DNP, APRN-CNP, focuses on a dietary intervention implemented by a nurse-practitioner-led team in a community setting. Research by Jie Hu, PhD, RN, FAAN, focuses on diabetes self-management interventions for African American adults with type 2 diabetes.
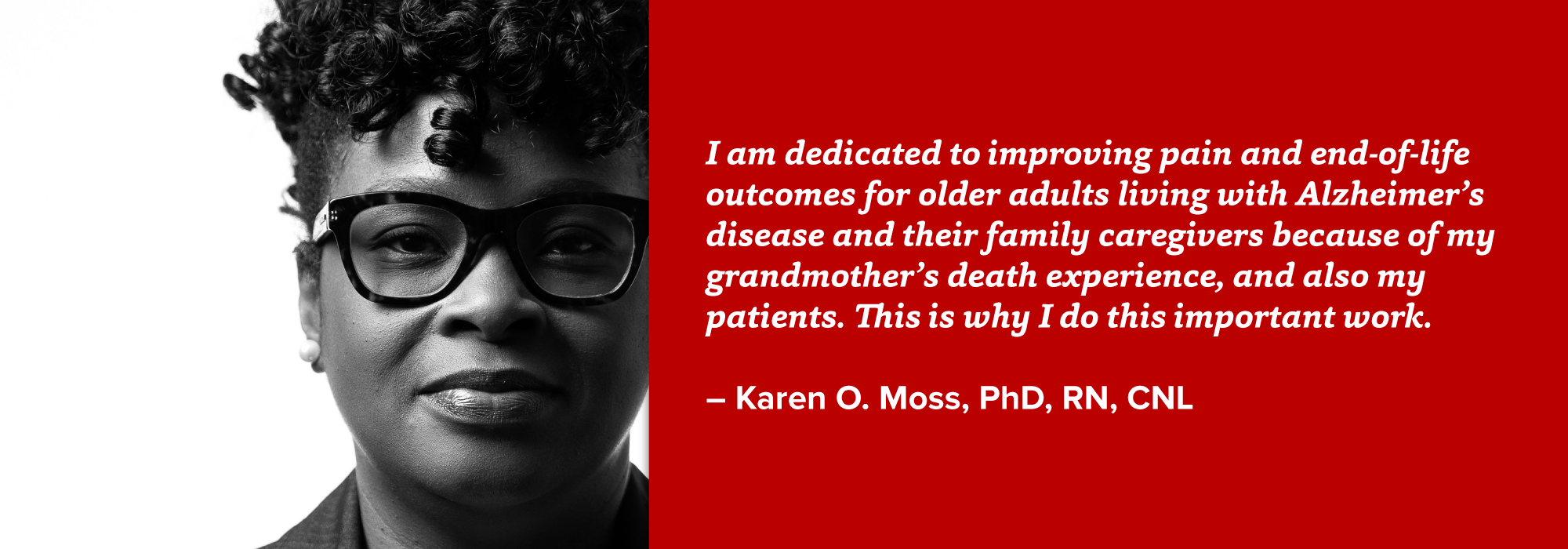
NIH diversity supplement grants, which allow researchers to add or highlight underrepresented populations in an existing study, help address disparities in healthcare. “Differences in Pain Among Blacks and Whites with Alzheimer’s Disease,” led by Karen O. Moss, PhD, RN, CNL, is a diversity supplement study funded by the National Institute on Aging (NIH/NIA) that will add new research questions to the study “Sex Differences in Pain Reports and Brain Activation in Older Adults with Alzheimer’s Disease” (Todd Monroe, PhD, RN-BC, FNAP, FGSA, FAAN, PI). Moss is also currently conducting a study on barriers and facilitators to advanced care planning as well as recruitment and retention with family caregivers of African American older adults living with dementia.
Where to go from here
Associate Dean for Research and Innovation and Nursing Distinguished Professor of Critical Care Research Mary Beth Happ, PhD, RN, FGSA, FAAN, stresses the importance of supporting our next generation of nurse scientists to carry on and expand this work. The research we have in progress currently is, she says, “a great start.” Many of these studies are early stage or in progress, and Happ cautioned, “One of the big challenges for us will be to shepherd these studies to their conclusion and dissemination.” We must continue to grow our research with diverse populations to see it to fruition and create maximum impact.
Our faculty researching solutions to problems of health equity
Support we have received to fund this research:
In this issue
- Improving Health Inequities Through Our Research
- Hotspot: New York City
- Going the Extra Mile
- From Sick Care to Well Care
- COVID-19 Challenges Inspire Solutions
- Caring & Creativity
- Evidence-based Practice
- Building Relationships with Olivia Cotton
- Young Alumni Blog
- Homecoming 2020
- Sandra Cornett
- Coping with COVID-19